National Center for Health Statistics: Birth Data Files
Jordan Peterson: Accidental Childlessness, The Epidemic That Dare Not Speak Its Name
REDDIT: An estimated 1/3 of all GenZ were aborted
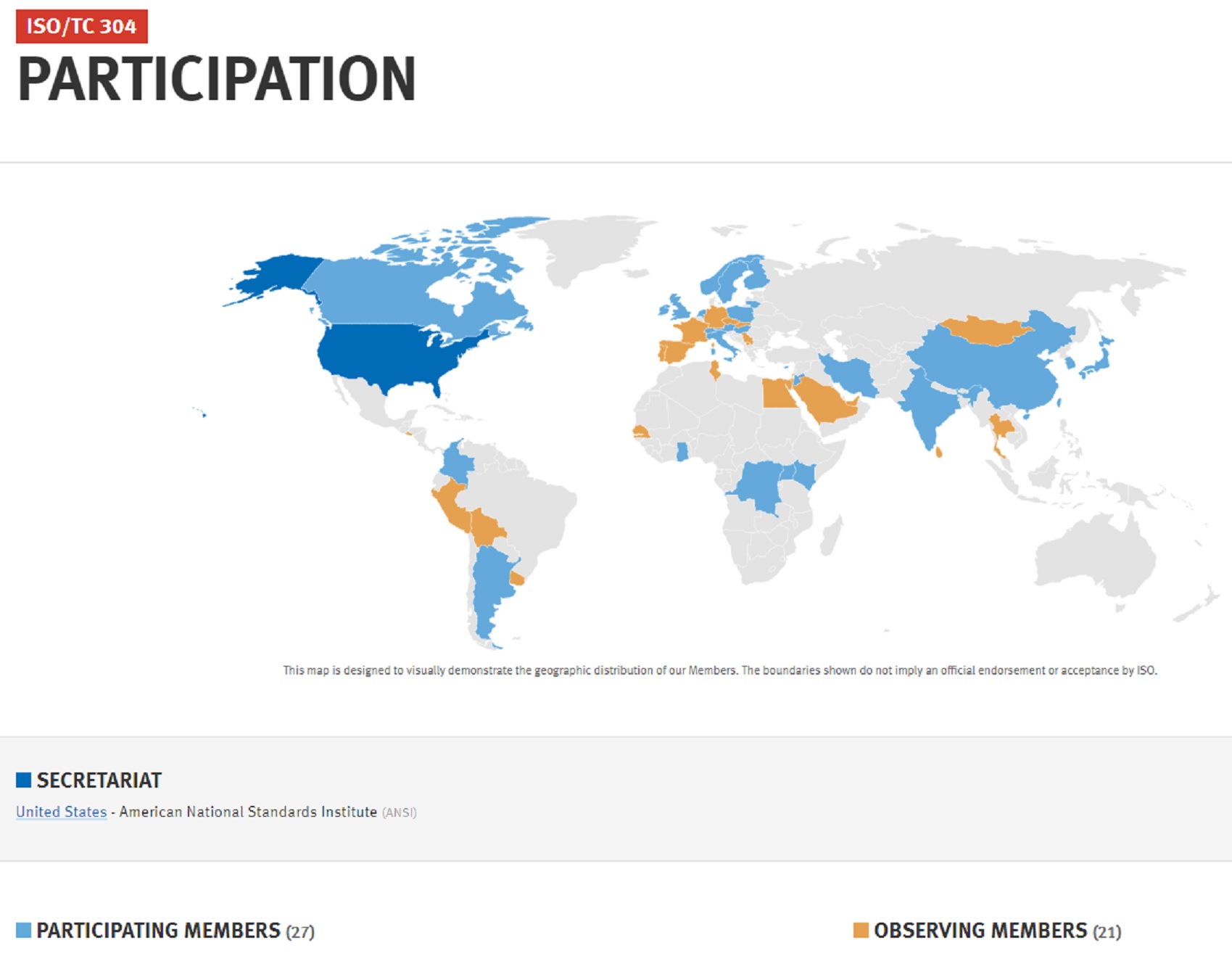
Today we break down the stack of regulations, codes, standards and open-source literature governing the safety and sustainability of university-affiliated medical research and healthcare delivery facilities. Because of the complexity of the topic we break down our coverage:
Health 200. Survey of all relevant codes, standards, guidelines and recommended practices for healthcare settings.
Health 400. All of the above with special consideration needed for obstetrics, gynecological and neonatal clinical practice and research.
We limit our interest to systems — water, power, telecommunication and security; for example — that are unique to campus-configured, city-within-city risk aggregations. Electrotechnologies (voltage stability, static electricity control, radio-interference, etc.) in these enterprises are subtle, complex and high risk. Sample titles from legacy best practice literature in this domain are listed below:
American College of Obstetricians and Gynecologists: Levels of Maternal Care
Provision of Care, Treatment, and Services standards for maternal safety
Since our interest lies in the habitable spaces for these enterprises we usually start with a scan of the following titles:
International Building Code Section 407 (Institutional Group I-2) identifies requirements specific to healthcare settings, covering aspects such as fire safety, means of egress, and smoke compartments. Maternity and obstetric facilities within hospitals fall under this classification.
K-TAG Matrix for Healthcare Facilities
NFPA 70 National Electrical Code Article 517
NFPA 99 Healthcare Facilities Code
NFPA 101 Life Safety Code Chapters 18 & 19
ASHRAE 170 Ventilation of Healthcare Facilities
Relevant Institute of Electrical and Electronic Engineers research
Towards Deeper Neural Networks for Neonatal Seizure Detection
A System to Provide Primary Maternity Healthcare Services in Developing Countries
Deep Learning for Continuous Electronic Fetal Monitoring in Labor
Reorganizing of University Hospital of Oran’s operating theatre: Simulation approach
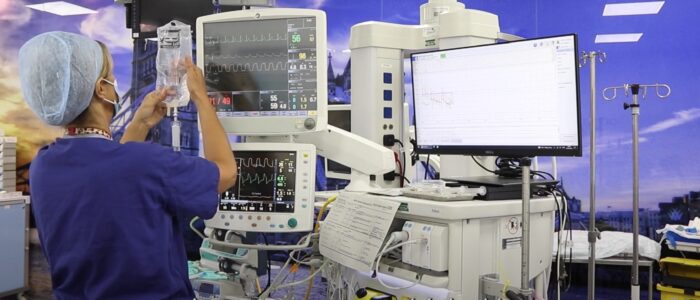
Finally, we collaborate with the IEEE E&H Committee on the following IEC committee projects from IEC/TC 62 Electrical equipment in medical practice:
– Common aspects of electrical equipment used in diagnostic imaging equipment
– Equipment for radiotherapy, nuclear medicine and radiation dosimetry
– Electromedical equipment for neonatal care
![]()
More
A relatively new publisher of related standards is the Facility Guidelines Institute. We are monitoring its catalog and its processes. The healthcare facility industry is likely large enough for another non-profit but we have yet to see meaningful leading practice discovery and promulgation that is unrelated to the literature that is already out there.
Health Insurance Portability and Accountability Act (HIPAA)
Health care cost as percentage of Gross Domestic Product for six representative nations.
Association of Academic Health Centers
International Conference on Harmonization: The ICH guidelines provide guidance on the development of pharmaceuticals and related substances, including clinical trials, drug safety, and efficacy.
Animal Welfare Act and the Institutional Animal Care and Use Committee
Good Laboratory Practice: GLP is a set of principles that ensure the quality and integrity of non-clinical laboratory studies. It ensures that data generated from non-clinical laboratory studies are reliable, valid, and accurate.
International Code Council Representation of Interests
In the early to mid-1900s, some US colleges used orphaned babies in home economics programs to teach child-rearing skills
These children were referred to as "practice babies" pic.twitter.com/FZCkeu0p2m
— UberFacts (@UberFacts) August 17, 2023
👩⚕️👩🎓 Warmest congratulations to UCD School of Nursing, Midwifery and Health Systems’ Higher Diploma in Midwifery group (2022-2024), who have officially completed their 18-month programme to become registered midwives 👏👏👏 pic.twitter.com/hixD1gT1no
— University College Dublin (@ucddublin) March 7, 2024